
After weeks of declining coronavirus deaths, the number of fatalities reported globally increased by 4%, according to the World Health Organization.
The U.N. health agency said there were 8,700 COVID-19 deaths last week, with a 21% jump in the Americas and a 17% increase in the Western Pacific.
WHO said coronavirus cases continued to fall, with about 3.2 million new cases extending a decline in COVID-19 infections since the peak in January. Still, there were significant spikes of infection in some regions, with the Middle East and Southeast Asia reporting increases of 58% and 33% respectively.
“Because many countries have reduced surveillance and testing, we know this number is under-reported,” WHO Director-General Tedros Adhanom Ghebreyesus said. He said there was “no acceptable level of deaths from COVID-19,” given that the global community now has the vaccines, medicines and diagnostics to stop the virus.
While many rich countries in Europe and North America have mostly dropped their virus restrictions, China’s extreme COVID-19 policies have meant more mass testing, quarantines and sequestering of anyone who was in contact with a case.
“We will probably never stop getting COVID,” said Matthew Miller, holder of the Canada Research Chair in viral pandemics at Hamilton’s McMaster University. How often we get reinfected will depend how quickly SARS-CoV-2 mutates in the future and how long immunity lasts, he said. “Both issues are a little bit uncertain at the moment,” though it’s possible to make some reasonable predictions, he said.
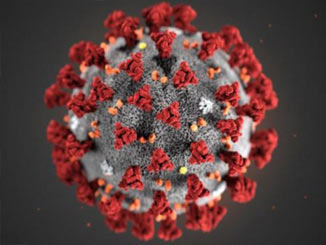
“Viruses like smallpox and polio (which can be eliminated) do not generate ‘variants’ capable of escaping immunity in the same way as coronaviruses,” said Miller. Alpha, Beta, Delta and then the remarkably contagious Omicron. The rapid-fire emergence of new variants has largely been driven by the “massive number of infections that have happened globally over the past couple of years,” Miller said.
Heavily mutated Omicron was more transmissible than Delta, and its subvariants BA.2, BA.4 and BA.5, appear more efficient spreaders still. The recent sixth wave was propelled by the BA.2 subvariant, and BA.1 infections didn’t entirely prevent people from getting reinfected with BA.2.
Unlike the measles, mumps and rubella vaccine that tends to be durable for life, antibodies induced by COVID-19 vaccines drop off. “There’s not a magic number; people round things up to three months, six months,” said Dr. Sameer Elsayed, a professor at Western University and a physician with London Health Sciences Centre. “You need more boosters to get your immune system strong and able to fight some of these variants that the vaccines weren’t initially made for.”
“We’re not necessarily recommending that everyone get fourth boosters or fourth doses,” he said. We’re hitting the tail end of Omicron, and, theoretically, too many boosters could over activate the immune system. “I don’t want people to misinterpret what I’m saying — we 100 per cent support vaccination,” Elsayed said.
Evidence from South Africa suggests the BA.4 and BA.5 Omicron subvariants, the fastest growing strains in the United States, the United Kingdom and other parts of the world, are able to dodge immunity from BA.2 infections. “We’re not seeing a lot of it yet (in Canada), so we’ve got our fingers crossed,” said Hankins, an epidemiologist and professor of public and population health at McGill University. “But for people who think, ‘It’s a done deal now, I’m giving up.’ This is not the time to give up. We still have quite a lot of the population that hasn’t been infected,” Hankins said. “You do not want to get an infection.” Statistics Canada reported a jump in excess deaths in January, and nobody wants to get long COVID if they can avoid it. “And every infection means the potential to transmit to other people who may be potentially more vulnerable than you to develop a severe outcome,” she said.
Dr. Deepta Bhattacharya wrote in The New York Times this week. Omicron and its subvariants tend to infect the upper respiratory tract, rather than deeper in the lungs, making symptoms less severe, and less serious still, even “nonexistent,” for the vaccinated and boosted.
“I think it’s reasonable to expect that, in general, infections will be much less severe than we observed early in the pandemic, because even if our immune responses do not provide perfect protection against reinfection, they do protect very well against severe illness,” Miller said. “As more people are vaccinated, infected, or combinations thereof, we will be increasingly protected as a population.” During the Omicron wave, the unvaccinated with a previous infection had a higher chance of getting reinfected, compared to the vaccinated. Omicron specific vaccines are due to be released by both Pfizer and Moderna.
There are still questions to be answered about long COVID and whether repeat infections increase the risk. It likely depends more on the severity of the infections rather than necessarily how many, Elsayed said. Whether re-infection can cause a rebound of long COVID in some people also isn’t entirely clear.
“It depends on the exposure. There’s not a lot of Omicron circulating around now compared to before,” Elsayed said. Omicron, which is transmitted through the air, is 100 times more contagious than the other virus everyone is talking about, monkeypox, which is not thought to be airborne. Hankins said it’s about living with COVID smartly: Assess the situation you’re in, decide when to wear a mask, when to avoid a crowded, poorly ventilated place. “Use your own judgment, and when you’re eligible for a dose of vaccine, get that vaccine because it will boost your immunity.”
“I think we should expect that evolution of new variants to slow down as the virus becomes endemic,” Miller said. “As rates of infection decline, the opportunity for new variants to emerge will also decline, which should prolong protection our immune system offers from re-infection.”

Leave a Reply